Why Am I Not Losing Weight?
So, you’re doing all the right things but still left wondering, “why am I not losing weight?”
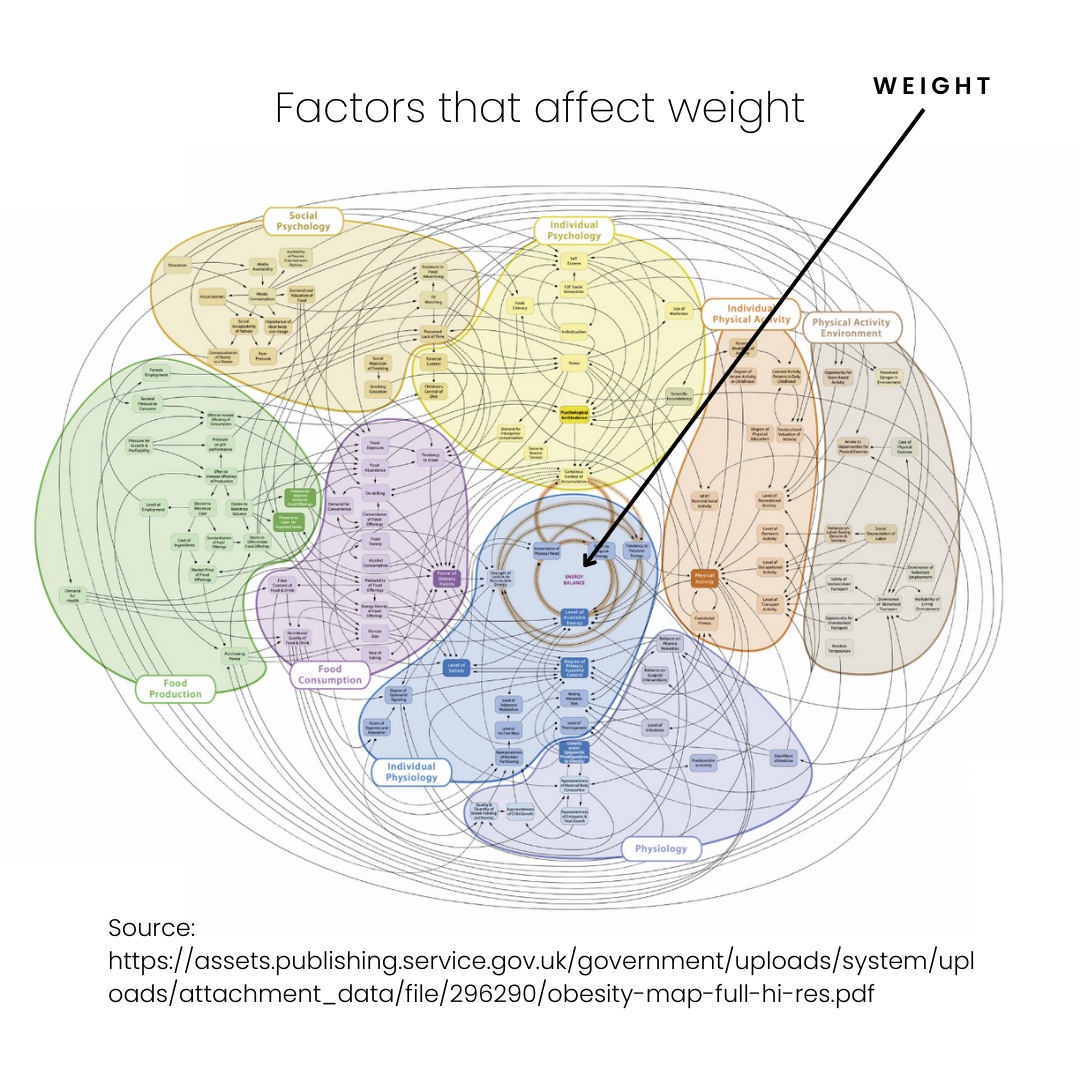
Weight loss is NOT as simple as Calories In < Calories Out
-
genetics
-
metabolism
-
stress & sleep
-
illness & disease
-
food intake
-
physical activity
- social & environmental factors
- age/life-stage
Top 5 reasons you’re not losing weight
As discussed above, weight is influenced by a myriad of factors. The factors discussed below are those which we see most commonly in our clinic. Please always discuss your individual concerns with your healthcare provider.
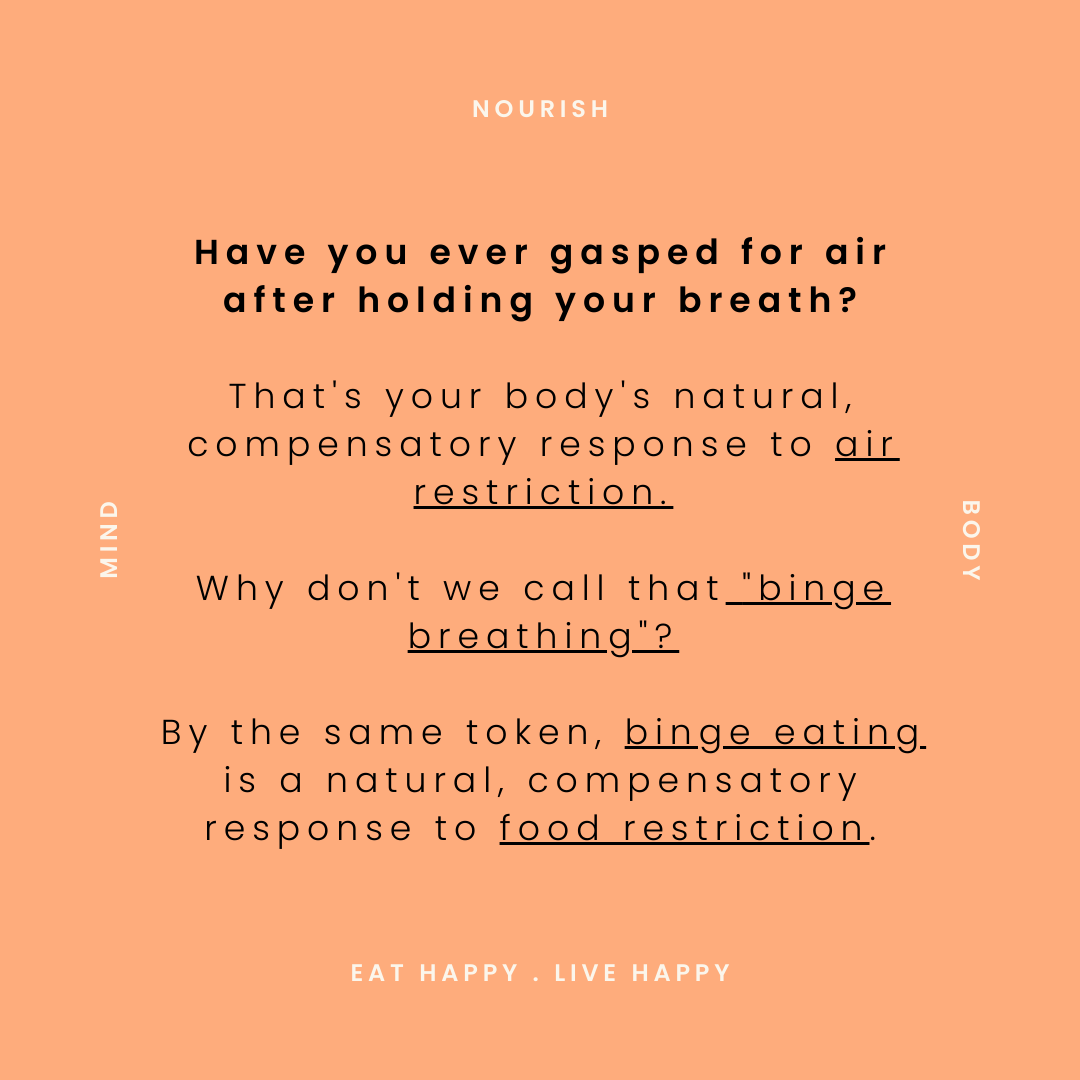
1. Restriction is leading your metabolism to slow down
3. You are struggling with binge eating
4. You’re focusing too hard on the numbers
5. There is something going on medically

How to not focus soley on weight loss
How has the persuit of weight loss affected your life thus far? Has it bought you the happiness and health that diet culture promises?
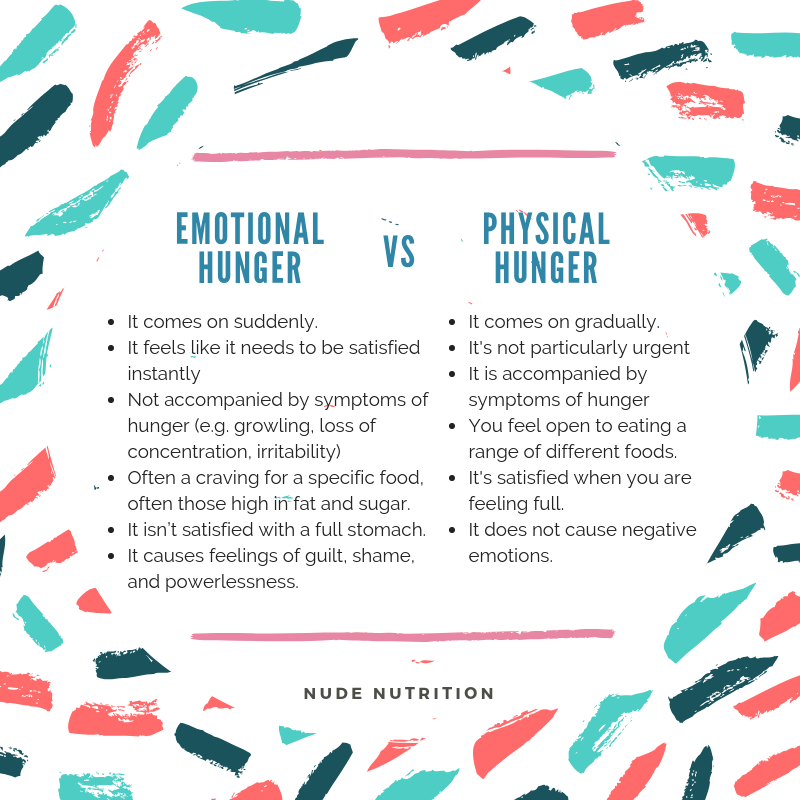
A big part of Intuitive Eating is relearning how to listen, and appropriately respond to hunger and satiety cues. This is really helpful when trying to stop counting calories. The freebie below has tips and tools that can help you get started with this.