Why do I eat if I’m not hungry?
Are you wondering “Why do I eat if I’m not hungry?”
We’ve all been there. You’re sitting on the couch after dinner and the next thing you know you’re in the fridge searching for something to round it off. Or you’re working hard on a deadline but can’t resist the urge to keep heading to the pantry for snacks. But all the time you’re thinking “I’m not even hungry”!
Should I only eat when I’m hungry?
The short answer is “no”. As humans, it’s very normal for us to sometimes eat when we’re not hungry.
You are not a robot! You have emotions to deal with, celebrations to attend, and friends to meet up with over brunch.
That being said…
Do you find yourself frequently eating to the point of feeling uncomfortably full? Maybe this leaves you feeling guilty or worried about what will happen to your weight. If so, this is something worth addressing. We will get into how further down the article.
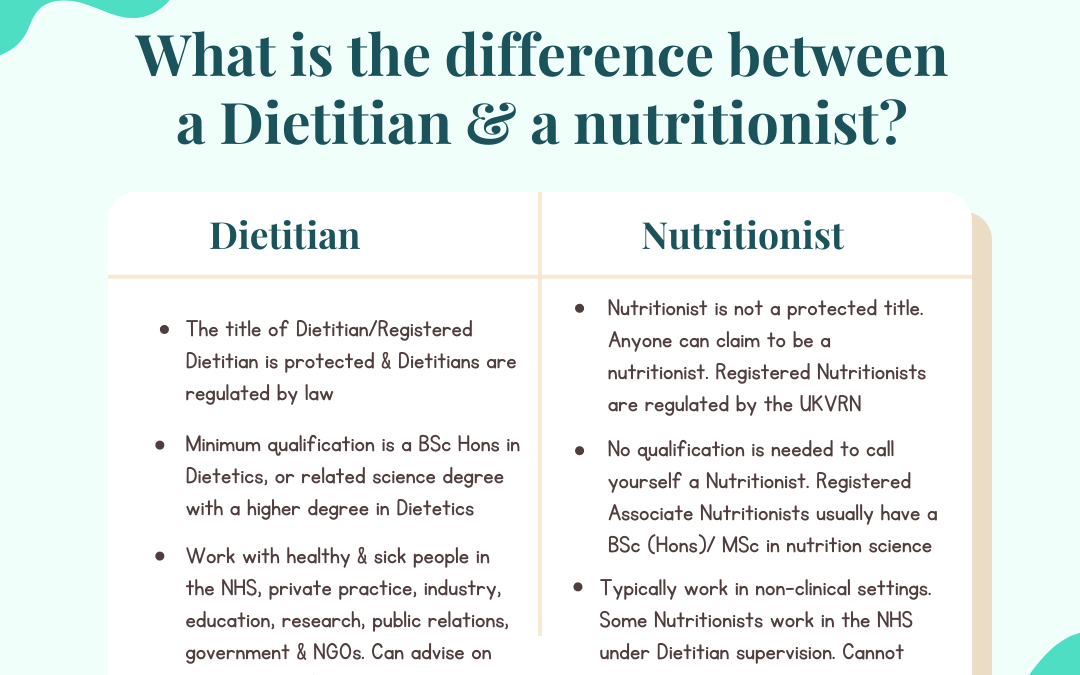
In my work as a Registered Dietitian and Certified Intuitive Eating Counsellor, I am all for listening to your body’s signals and “eat when you’re hungry, stop when you’re full”. But too often this can get twisted into a hard and fast rule (which it was never meant to be). This can really mess with our heads and become another form of restrictive eating that keeps us stuck in an unhealthy relationship with food.
Pssst…are you sure it’s not physical hunger?
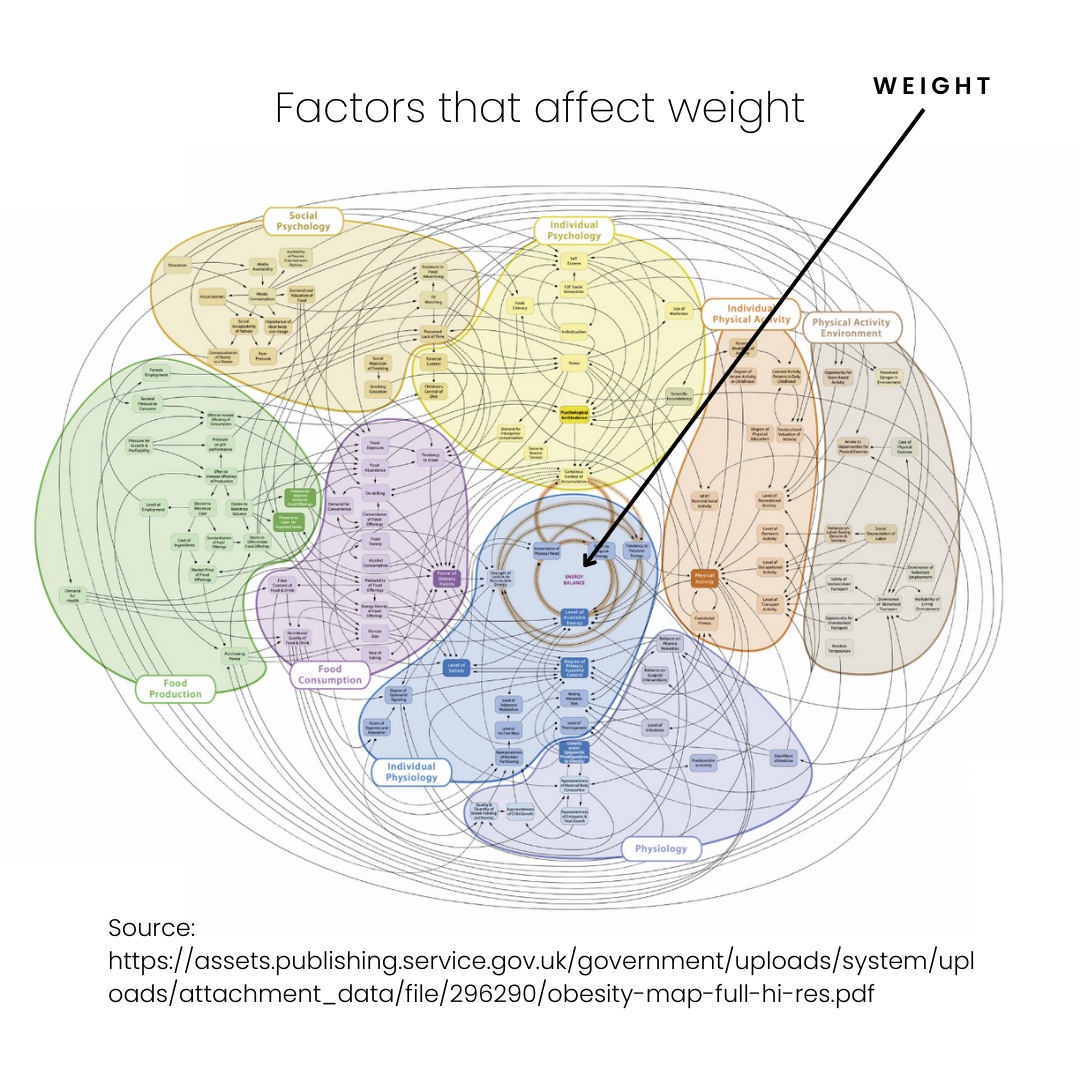
I see it so often with my clients… they tell me they are emotional eaters or addicted to sugar. But actually, when we dive into it, years of living in diet culture has warped their idea of what a healthy amount of food is.
We are sold an idea that we should be able to subsist on 1200-1500kcal/day and then wonder why are feeling out of control around food!
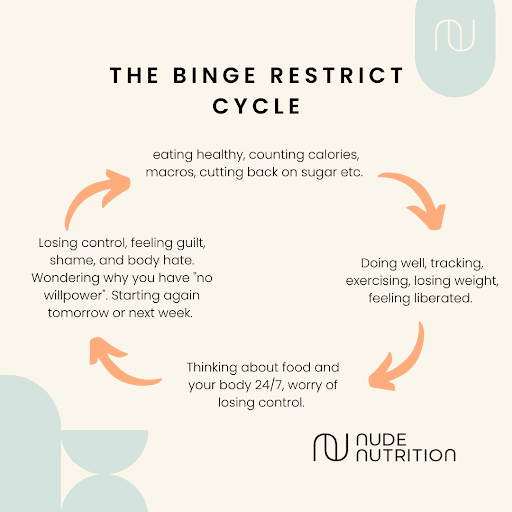
Is it possible that you are just not eating enough food throughout the day through restriction (trying to lose or maintain weight), or just busyness? If so, by the time the evening comes, there can be a primal drive to want to eat which can induce nighttime binges. That judgy voice can then creep in, labelling it as an ‘emotional’ or ‘comfort’ eating episode, which is also judged as ‘bad’. When actually you were just genuinely hungry because your body has been needing fuel all day. This can trigger compensatory behaviour, such as restriction or over-exercise to ‘make up’ for it. Restriction usually only exacerbates the cycle of overeating at some point later to happen again.
Sound familiar? If so, Intuitive Eating is a framework I use with clients that can help them figure out how to eat enough throughout the day to prevent this from happening. More on this below.
If you’re pretty sure you’re eating adequately and still left wondering “Why do I eat if I’m not hungry?”….here are some other factors that could be playing a role.
5 reasons you may eat when you’re not physically hungry
1. You want the taste
Taste hunger occurs when you are craving a specific food. This can accompany physical hunger or occur when you are not physically hungry. Basically, taste hunger is when a food just sounds good! It’s really normal to have the desire for a little something to round off your meal and provide the “satisfaction factor”. Like sweets, biscuits, ice cream, fruit, yoghurt, hot chocolate etc. This is not bad, and it’s not emotional eating. If you’re feeling the desire to eat something sweet after your meal, maybe that’s just what you need to hit the satisfaction factor.
If you’ve identified that you’re 100% not physically hungry, it’s not taste hunger, you have worked on making peace with food and no amount of food will fill you up, then it’s likely that you’re experiencing emotional hunger.
It’s really normal to have the desire for a little something to round off your meal and provide the “satisfaction factor”.
2. You’re experiencing uncomfortable emotions
Do you find yourself eating when bored, procrastinating, lonely or anxious?
Again, it can be normal to turn to food sometimes for comfort. However, if food is your main coping mechanism for dealing with tough things, and it’s causing you distress, this is something worth addressing.
Emotional eating is really common and something we see often with clients. For strategies and information on how to address emotional eating see my other article: How to Navigate Emotional Eating
Are you someone who actively tries to avoid “bad food”, but then when you’re bored, stressed, or lonely, find yourself uncontrollably diving into all of the foods you’re trying to avoid? Sometimes emotions get in the way and interfere with your restriction. It’s a backlash effect of the restriction. Interestingly, research shows that former or current dieters have higher emotional eating than people without a history of dieting. Basically, dieting (any pursuit of weight loss) can exacerbate emotional eating.
3. You’re full, but you’re not satisfied
There is a difference between feeling physically full versus being satisfied with food. For example, if you eat enough garden salad you will eventually feel full from the sheer volume of food in your belly, but you probably won’t feel satisfied. This can leave you hankering for more food and wondering “Why do I eat if I’m not hungry?”.
As well as physically filling you up, your meals and snacks need to mentally and physically satisfy you so that you do not feel restricted (remember: restriction leads to deprivation and more thinking about food). This means choosing foods that we crave or that “hum” to us. If you’re craving a crispy pizza but opt for soup, you’re unlikely to feel satisfied.
To ensure physical satisfaction, I often talk about the importance of choosing options with “staying power” with my clients. These are usually those which include a source of each fat, protein, carbohydrate, and fibre.
4. Your restrictive eating is having a backlash effect
Are you trying to not eat certain foods to be healthier or lose weight? Perhaps you’re trying to cut back on carbs, fatty foods, sweets and chocolates. If this sounds like you, it could be paradoxically making you eat MORE of these foods when you’re not even hungry.
Annoying huh?! But that’s just the way our human brains are wired. Research on thought suppression tells us about this. Thought suppression is intentionally trying not to think about something (i.e. a plate of chips or a creamy bar of chocolate). A large body of research indicates that thought suppression is ineffective. Moreover, it can lead us to think more about the very thing we are trying not to do. Imagine being told, “Don’t think of a pink bear.” This is an example of thought suppression. Give it a try—close your eyes for a minute and try not to think of a pink bear. What happens?
The solution? It’s to allow yourself permission to eat ALL foods. When we allow ourselves this permission we are likely to eat these so-called “naughty” foods in more moderate amounts and feel more in control around them.
This can sound scary or you may be doubting if it will work for you. My free guide below will walk you through the process.
5. It’s a habit
Reaching for a snack when you walk through the door? Automatically grabbing something sweet after dinner? Mindlessly munching in front of the TV?
A lot of our eating behaviours are automatic. And there’s nothing inherently wrong with this. But if you’re finding these habits are leaving you feeling sluggish or uncomfortably full, intuitive eating strategies can help.
Try bringing more awareness to the habitual eating occasion that’s bothering you by:
- Check-in with your hunger level prior to eating (this doesn’t mean you can’t eat if you’re not hungry, it just means you get to make the conscious choice)
- If you’re not hungry – can you label what you are feeling? Ie. are you bored, lonely, or procrastinating on a task that needs doing?
- Sit down to eat in a pleasant environment, without screens
- Remain present with the sensory experience of eating the food (ie. what does it taste, smell and feel like when you’re eating?)
All these strategies help us stay mindful of the eating experience and interrupt unhelpful behaviours that aren’t serving us.
How do I train myself to eat intuitively?
Intuitive eating is a tool that can help you learn the difference between physical hunger and emotional hunger. It can help you understand why you eat when you’re not hungry.
Intuitive Eating is an evidence-based approach to help improve your relationship with food and have better self-control around food. This framework can help you learn to honour your health by listening and responding to the messages of your body. This helps you to meet your physical and mental needs based on your terms and move away from external diet tools such as the time of day, points systems, calorie tracking, rigid rules or meal plans – which can all make us more likely to eat when food isn’t really what’s going to satisfy us. You can learn more about Intuitive Eating here.
Another great place to start is my free guide which runs through some of the key principles of Intuitive eating.
Want more individualised support? I run a private practice with a team of Dietitians and a Psychotherapist, to help you navigate your way to a more balanced and nourishing relationship with food. You can find out more about that here. and get in touch for a free 20-minute discovery call.