Is Online Nutrition Coaching Worth It? What To Expect From Personalised Support
If you have had a tough year with food rules, guilt, or body worries, you might be wondering whether online support is really worth it. You want help that is personal and evidence-based. You want to feel calmer around food, not more restricted. As the holidays draw closer, with social meals and shifting routines, it makes sense to ask whether online nutrition coaching can give you the support you need, wherever you are.
This guide walks you through what an online nutrition coach actually does, how personalised it can be, what you can expect to pay, and how it compares with in-person care. You will also hear how clients at Nude Nutrition have used remote coaching to step away from shame, rebuild trust with their bodies, and feel more at ease during moments that used to feel chaotic.
Before understanding how coaching works, you might be wondering how to find someone qualified. This article on what to look for in an online Nutritionist or Dietitian tackles that question.
What an online nutrition coach actually does
A qualified online non-diet nutrition coach helps you make peace with food and reconnect with your body’s cues through structured, compassionate guidance. At Nude Nutrition, sessions are delivered by Registered Dietitians and Intuitive Eating Counsellors.. You meet via secure video calls, discuss your history and goals, and create a plan that fits your life. The focus is not weight-loss targets or strict rules. The focus is on healing your relationship with food, understanding hunger and fullness, and building confidence to eat in a way that feels sustainable.
Here is what this looks like in practice:
- Gentle assessment of current patterns, health background, and goals.
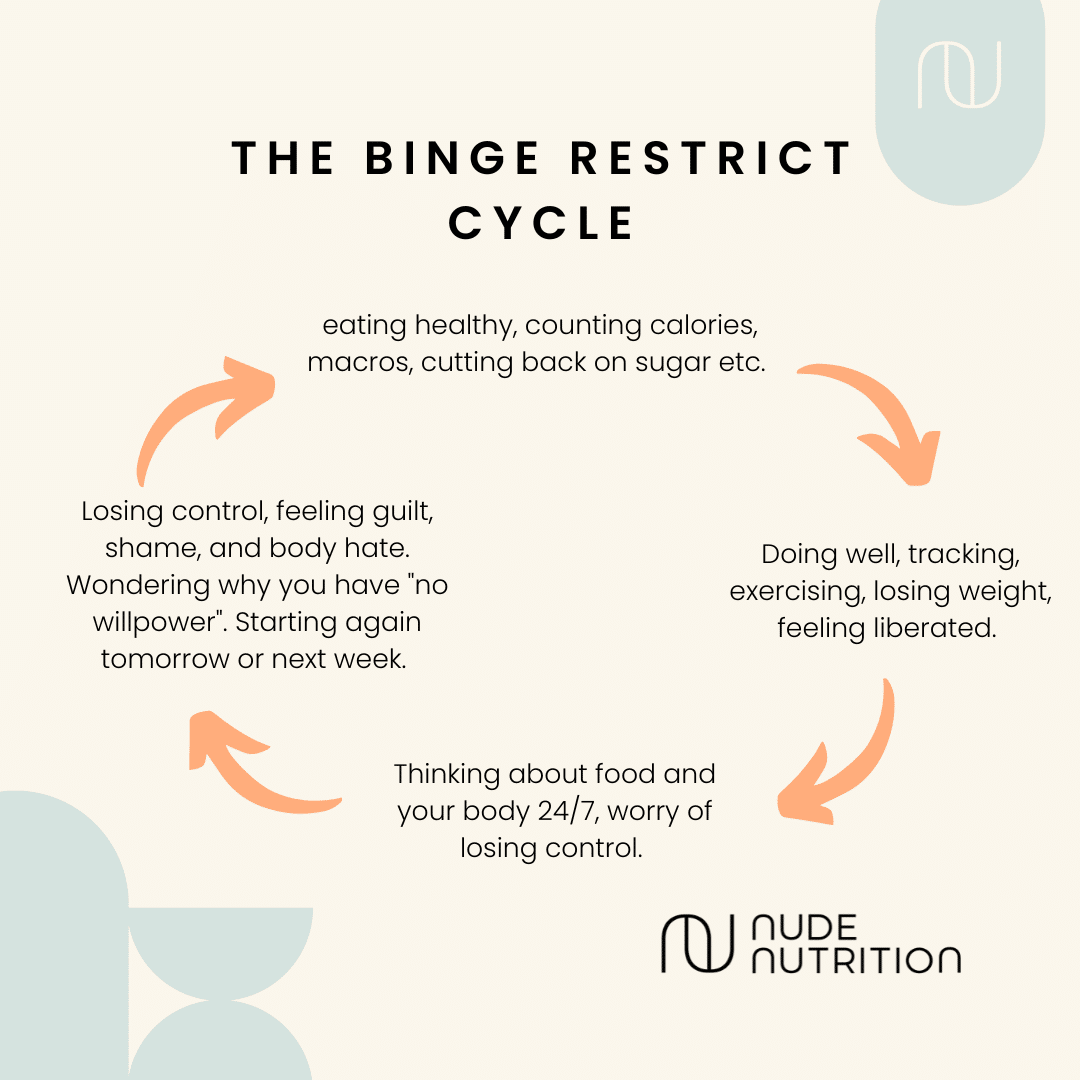
- Clear, kind education about why diets and rigid rules backfire, with a science-based approach rooted in intuitive eating and Health at Every Size principles.
- Personalised experiments to reduce binges and soothe night-time eating, including exploring whether you are eating enough during the day, and whether your meals are satisfying.
- Practical strategies for emotional eating that replace self-criticism with coping skills and self-compassion.
- Ongoing messaging support between sessions during office hours for questions and encouragement.
Clients often arrive worried that they are the problem, that they lack willpower, or that they should just try harder. A qualified non-diet nutrition coach can reframe the issue. If you are overeating at night, for example, we explore whether daytime restriction or unsatisfying meals are driving biological hunger later on, then we build a pattern that steadies your energy and mood.
How personal is online support?
Very personal. You meet one-to-one with a Registered Dietitian and Intuitive Eating Counsellor who learns your history, your triggers, and your values. You co-create goals that make sense for your life. If you live with IBS, PCOS, diabetes, or a history of disordered eating, your support will reflect that. If you fear “losing control” at parties, we plan for that with practical steps and language you can use with friends and family.
Support continues between sessions. You can share reflections, ask for help before a challenging event, and celebrate wins after. Many clients say this is where real change happens, since the support lands exactly when emotions and decisions are live.
One client told us she used to avoid dinners out because she feared she would spiral afterward. With the right support and coaching, she learned to eat enough earlier in the day, added foods she actually enjoyed, and practised non-judgement after meals. Over a few weeks, her anxiety faded, and she started to enjoy evenings again.
Is online nutrition coaching worth it?
If you want to stop cycling through restriction and rebound eating, if you feel trapped by food guilt, and if you want a calmer relationship with your body, online coaching is often worth it. The value comes from:
- Accessibility, you can meet from home, which means fewer cancellations and more consistency.
- Personalisation, plans align with your schedule, health needs, culture, and preferences.
- Continuity, in between support helps you apply tools in real life.
- A non-diet focus, you learn skills that last, not rules you abandon after a tough week.
- Clients report fewer binge episodes, less anxiety about social eating, improved digestive comfort, and a kinder inner voice. Many tell us they finally enjoy holidays without the familiar swing from strict control to feeling out
of control.
That said, it should be the right fit. If you want a quick fix or a meal plan that tells you exactly what to eat each day, this approach may frustrate you. If you are seeking long term change and you are open to trying small, realistic experiments, you will likely find it valuable.
Pros and cons vs. in-person support
Pros of online care:
- Convenience, no travel, easier scheduling, more privacy.
- More frequent touch points, messaging support can fill the gaps between sessions.
- Wider access to specialists, you can work with a Registered Dietitian and Intuitive Eating Counsellor who truly understands disordered eating, even if you do not live nearby.
Potential drawbacks:
- You may miss the feel of being in a shared room; some people prefer that presence.
- If your internet connection is poor, sessions can be disrupted.
- For acute medical risk in eating disorders, in-person multidisciplinary care may be required.
- We can collaborate with your GP or therapist to make sure you are supported safely.
What does an online nutritionist session include?
A typical Nude Nutrition programme starts with a thorough assessment to understand your history, health, and goals. You then meet regularly for 50 minutes to review progress, troubleshoot obstacles, and learn new tools.
We focus on:
- Rebuilding hunger and fullness awareness.
- Reducing all or nothing thinking.
- Planning satisfying meals that remove the need to “make up for” food later.
- Managing emotional eating with self-compassion rather than restriction.
- Addressing body image concerns with practical skills and gentle mindset work.
Between sessions, you have access to resources and Registered Dietitian and Intuitive Eating Counsellor contact during office hours. We also offer flexible scheduling, including evenings so support fits around your life.
How much does it cost to see an online nutritionist?
Pricing varies based on the length of support you choose, your clinician, and whether you book a package or one-off sessions. At Nude Nutrition, we offer multi-month programmes with set numbers of 50-minute sessions, plus messaging between sessions. There is a short discovery call and an initial consultation included in the programme fee. Payment plans are available, and we offer scholarship options for those with financial hardship. If you are unsure what you need, we can start with an initial consultation and build from there.
If you live with an active eating disorder, we will work alongside your healthcare team and ensure the format and frequency of sessions match your clinical needs.
Two simple steps you can try today
Add a satisfying afternoon snack. If evenings feel out of control, try a balanced snack with protein and carbs around 3 to 4 pm, then notice whether your night feels steadier.
Practise a pause, not a rule. Before you eat in response to stress, take three slow breaths, label the feeling, and decide your next step with kindness. No judgement, just data.
Where to learn more
If you are curious about support and want a feel for our approach, you can read about our online nutrition coaching. If you are ready to explore how to stop food obsession, we share gentle, practical steps you can try now. You can also book time to talk about online nutrition advice, through your goals and options before getting started.
Final thoughts
Online nutrition coaching is not another diet. It is personal, flexible, and grounded in evidence. If you want to feel calmer with food, rebuild trust in your body, and approach the holidays with more ease and less noise, it can be a powerful investment. Whether you need help unpicking emotional eating, finding steady rhythms through the week, or softening harsh self talk, you do not have to do this alone. We are here to help you heal your relationship with food and find a way of eating that feels like yours.